Here is a description of HCM from the article of Dr. Ali Marian and Dr. Eugene Braunwald “Hypertrophic Cardiomyopathy: Genetics, Pathogenesis, Clinical Manifestations, Diagnosis, and Therapy”:
Hypertrophic cardiomyopathy (HCM) is a genetic disorder that is characterized by left ventricular hypertrophy unexplained by secondary causes, and a non-dilated left ventricle with preserved or increased ejection fraction. It is commonly asymmetric with the most severe hypertrophy involving the basal interventricular septum. Left ventricular outflow tract obstruction is present at rest in about one third of the patients, and can be provoked in another third. The histologic features of HCM include myocyte hypertrophy and disarray, as well as interstitial fibrosis. The hypertrophy is also frequently associated with left ventricular diastolic dysfunction.
Let’s try to translate that into a more understandable language, shall we?
Genetics of HCM
Let’s break down how gene mutations can cause HCM:
Normal Instructions: Our bodies have instructions (genes) that tell our cells how to make proteins, which are like the building blocks for our body.
Mutations: Sometimes, there can be mistakes or changes (mutations) in these instructions. In the case of HCM, there are specific gene mutations related to proteins in the heart muscle.
Protein Production: These mutations cause the cells in the heart muscle to produce abnormal proteins. Instead of working as they should, these proteins can make the heart muscle cells grow too much.
Thicker Heart Walls: As a result, the walls of the heart become thicker, a condition known as hypertrophy. This can make it harder for the heart to pump blood effectively, leading to problems like shortness of breath or chest pain.
So, in simple terms, gene mutations in HCM lead to the production of abnormal proteins that cause the heart muscle to become thicker, making it more challenging for the heart to do its job properly.
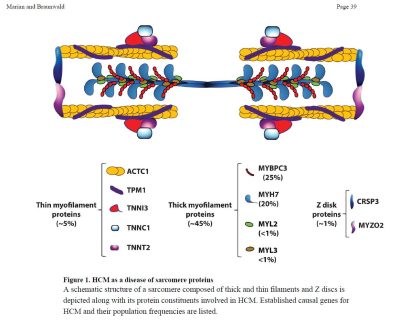 Involved genes: Among the known causal genes, MYH7 and myosin binding protein C (MYBPC3) are the two most common, together being responsible for approximately half of the patients with familial HCM. Mutations TNNT2, TNNI3, and TPM1 are relatively uncommon causes of HCM and together are responsible for less than 10% of cases. Mutations in ACTC1 (cardiac α-actin), MYL2 (myosin light chain 2), MYL3 (myosin light chain 3), and CSRP3 (Cysteine and Glycine Rich Protein 3) are also established, albeit uncommon, causes of HCM. Evidence for the causal role of the above nine genes in HCM is the strongest.
Involved genes: Among the known causal genes, MYH7 and myosin binding protein C (MYBPC3) are the two most common, together being responsible for approximately half of the patients with familial HCM. Mutations TNNT2, TNNI3, and TPM1 are relatively uncommon causes of HCM and together are responsible for less than 10% of cases. Mutations in ACTC1 (cardiac α-actin), MYL2 (myosin light chain 2), MYL3 (myosin light chain 3), and CSRP3 (Cysteine and Glycine Rich Protein 3) are also established, albeit uncommon, causes of HCM. Evidence for the causal role of the above nine genes in HCM is the strongest.
Mutations in TTN (titin), TCAP (telethonin), MYOZ2 (myozenin 2), TRIM63 (ubiquitin E3 ligase tripartite motif protein 63 or MuRF1) and FHL1 (four and a half LIM domains 1) also have been implicated as causes of HCM, but occur typically in sporadic cases and small families.
Approximately 60% of patients with HCM have a clearly recognizable familial disease.
Is HCM a disease specific for certain groups? No. HCM is a disorder without a distinct geographic, ethnic, or sex pattern of distribution. Prevalence of HCM has been estimated at 0.16% – 0.29% (~ 1:625 to 1:344 individuals) in the general adult population.
How is the HCM gene passed? If a parent has a gene mutation causing HCM, they can pass that mutated gene to their children when they have babies. Each child has a 50-50 chance of inheriting the mutated gene. It’s like flipping a coin – it can land on heads (with the mutation) or tails (without the mutation).
It’s important to note that not everyone with HCM got it from their parents. Sometimes, the gene mutation can happen for the first time in a person, and they become the first in their family to have it.
Glossary of terms
Alcohol septal ablation is a cardiac catheterization technique designed to reduce the obstruction to blood being ejected from the heart. The technique creates a small controlled myocardial infarction, killing the area of heart muscle responsible for the obstruction and eventually causing it to fibrose and become less thick. The technique is similar to coronary angioplasty and utilizes similar equipment. Wires and balloons are used to localize the septal artery feeding the diseased muscle under both fluoroscopic (X-ray) and echocardiographic (ultrasound) guidance, then a small amount of pure alcohol is infused into the artery to produce a small heart attack.
Angiography or arteriography is a medical imaging technique used to visualize the inside, or lumen, of blood vessels and organs of the body, with particular interest in the arteries, veins, and the heart chambers. This is traditionally done by injecting a radio-opaque contrast agent into the blood vessel and imaging using X-ray-based techniques such as fluoroscopy.
Atrial fibrillation (AF or A-fib) is an abnormal heart rhythm (arrhythmia) characterized by rapid and irregular beating of the atrial chambers of the heart. It often begins as short periods of abnormal beating, which become longer or continuous over time. It may also start as other forms of arrhythmia such as atrial flutter that then transform into AF. Episodes can be asymptomatic. AF may happen in brief episodes, or it may be a permanent condition.
Beta blockers (beta-blockers, β-blockers, etc.) are a class of medications that are predominantly used to manage abnormal heart rhythms and to protect the heart from a second heart attack (myocardial infarction) after a first heart attack (secondary prevention). They are also widely used to treat high blood pressure (hypertension), although they are no longer the first choice for initial treatment of most patients. Some widely used beta blocker brands are Atenolol, Bisoprolol, Metoprolol, and Nadolol.
Calcium channel blockers (CCB), calcium channel antagonists or calcium antagonists are a group of medications that disrupt the movement of calcium (Ca2+) through calcium channels. Calcium channel blockers are used as antihypertensive drugs, i.e., as medications to decrease blood pressure in patients with hypertension. CCBs are particularly effective against large vessel stiffness, one of the common causes of elevated systolic blood pressure in elderly patients. Calcium channel blockers are also frequently used to alter heart rate (especially from atrial fibrillation), to prevent peripheral and cerebral vasospasm, and to reduce chest pain caused by angina pectoris.
Disopyramide (trade names Norpace and Rythmodan) is an antiarrhythmic medication used in the treatment of ventricular tachycardia. It is a sodium channel blocker and therefore classified as a Class 1 antiarrhythmic agent.
An echocardiography, echocardiogram, cardiac echo – or simply an echo – is an ultrasound of the heart. It is a type of medical imaging of the heart, using standard ultrasound or Doppler ultrasound.
Electrocardiography is the process of producing an electrocardiogram (ECG or EKG). An electrogram of the heart is a graph of voltage versus time of the electrical activity of the heart obtained by using electrodes placed on the skin. These electrodes detect the small electrical changes that are a consequence of cardiac muscle depolarization followed by repolarization during each cardiac cycle (heartbeat). Changes in the normal ECG pattern occur in numerous cardiac abnormalities, including cardiac rhythm disturbances.
An implantable cardioverter-defibrillator (ICD) or automated implantable cardioverter-defibrillator (AICD) is a device implantable inside the body, able to perform cardioversion, defibrillation, and (in modern versions) pacing of the heart. The device is therefore capable of correcting most life-threatening cardiac arrhythmias.
Septal myectomy is a cardiac surgery treatment for hypertrophic cardiomyopathy (HCM). The open-heart surgery entails removing a portion of the septum that is obstructing the flow of blood from the left ventricle to the aorta.
Obstruction – depending on whether the distortion of normal heart anatomy causes an obstruction of the outflow of blood from the left ventricle of the heart, HCM can be classified as obstructive or non-obstructive.
A septum (Latin for something that encloses; plural septa) is a wall, dividing a cavity or structure into smaller ones. The heart septum divides its left and right side.
Treatments for HCM
We are living in a new, exciting era in the discovery of new HCM treatments. Until recenly all one could do was to manage HCM symptoms in one of the following manners:
1. Medications:
2. Surgical Procedures:
These surgical procedures need to be performed by experienced surgeons in high-volume centers.
3. Implantable Devices:
4. Lifestyle Modifications:
5. Regular Monitoring:
Last years, however, brought new exciting possibilities for treating the underlying condition itself. In 2023 the European Commission approved Camzyos (with active substance mavacamten) for use in the European Union with obstructive HCM patients. The molecule is a myosin inhibitor, promoting an energy-sparing and super-relaxed state that translates as a reduction in LVOT obstruction and improvement of cardiac filling pressures. Camzyos is owned and distributed by Bristol Myers Squibb. A molecule with a similar action, aficamten, is currently (as of end of 2023) in late stage trials for both obstructive and non-obstructive forms of HCM. Cytokinetics, the company that had developed aficamten, expects approval in 2024. Small-molecule treatments have shown excellent results in patients, acting as a viable alternative to surgical solutions to obstructive HCM.
Another exciting trend is the emergence of gene therapies. For example, Tenaya Therapeutics in early 2023 initiated a Phase 1 study of TN-201, an adeno-associated virus (AAV)-based gene therapy designed to treat adults and children with HCM due to MYBPC3 gene mutations, the most prevalent form of genetic HCM. The therapy is intended to address the underlying cause of disease by delivering a fully functional MYBPC3 gene to restore normal levels of MYBPC3 protein with the hope of potentially halting disease progression and reversing the course of genetic HCM after a single treatment!